Featured Articles
Items filtered by date: April 2022
Tuesday, 26 April 2022 00:00
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Tuesday, 26 April 2022 00:00
What Is a Heel Spur?
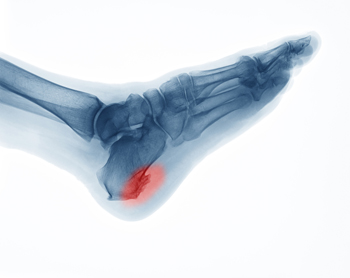
When the heel bone suffers repeated strain or irritation, the body can react by sending extra amounts of calcium to the injury site to protect it. Among the causes are poorly fitting shoes, obesity, arthritis, gait abnormalities, excessive running, and plantar fasciitis. This calcium can build up over time and cause hard, pointy deposits, known as spurs, to develop on the heel bone. Heel spurs can cause pain that may be worse in the morning or more mild and steady throughout the day. Rest or activity can trigger the pain. Heel spurs may occur along with plantar fasciitis, which may cause tenderness and inflammation as well. Not all heel spurs are painful, but those that are can be treated by a podiatrist with a variety of therapies including custom orthotics, physical therapy, cortisol injections, anti-inflammatory medications, or surgery if more conservative methods do not provide relief.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of the podiatrists from JE Foot & Ankle Associates. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the latest in diagnostic and treatment technology to meet your needs.
Wednesday, 20 April 2022 00:00
Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes, peripheral vascular disease, neuropathy, cancer, and severe crush injury. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If the bone is removed, it is then replaced with prostheses, synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
Wednesday, 20 April 2022 00:00
How You Can Protect Your Limbs as a Diabetic
While complications of diabetes, such as poor circulation and neuropathy, can make a wound easier to develop and harder to detect and heal, there are many preventative measures you and your podiatrist can take to reduce your risk of amputation. On your end, make foot care a priority. Wear shoes and socks that fit well and don’t rub against any part of your feet or cut off circulation. Avoid walking barefoot. Elevate your feet and wiggle your toes frequently to keep the blood flowing. Eat a balanced diet and exercise to help manage your sugar levels and maintain a healthy body weight. Don’t smoke. Inspect your feet twice a day, using a mirror if needed, to see the bottom of your feet. Get to your podiatrist right away if you spot anything unusual. Early recognition/treatment of a problem can greatly reduce your risk of amputation. Some wounds may be avoided by getting regular foot screenings and having a podiatrist trim your toenails and treat any corns or calluses. They may also prescribe diabetic shoes and create custom orthotics to prevent foot injuries. If a wound does develop, your podiatrist can dress your wound appropriately, remove dead skin and tissue (debridement), reduce pressure and friction on the wound, and help restore adequate blood flow. They can also advise you on how to properly care for your wound at home. In cases where a higher level of wound care is necessary, your podiatrist may be able to use skin or bone grafts, or perform reconstructive surgery to replace or rebuild infected or necrotic bones, tendons and tissue.
Limb salvage can be an effective way in preventing the need for limb amputation. If you have diabetes, cancer, or any other condition that could lead to foot amputation if left unchecked, consult with one of the podiatrists from JE Foot & Ankle Associates. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Limb Salvage?
Limb salvage is the attempt of saving a limb, such as the foot from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Diabetes is the number one cause of non-traumatic amputations in the United States. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
However, there are other causes as well, such as cancer and traumatic injury. Links between higher mortality rates and amputation have been found. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Tuesday, 12 April 2022 00:00
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Tuesday, 12 April 2022 00:00
Your Feet and Falling
Falling can result in bone breaks or worse, and they are especially prevalent among older people. While there are many causes of falls, such as poor eyesight, hearing, slowing of reflexes, or side effects from medication, foot problems can also impact balance and gait and result in falls. Those with diabetes or circulatory problems need to be particularly careful to examine their feet for problems they might not feel. Simple things one can do to help avoid falling include checking environments for safety hazards, wearing properly fitted and supportive footwear, staying physically active, having regular examinations of ears and eyes, limiting alcohol consumption, using canes or other assistive devices if called for, and being aware of unusual ground conditions. Meeting with a podiatrist to check your feet, help assess risks for falls, and inform you of how to minimize this from happening in the future.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of the podiatrists from JE Foot & Ankle Associates. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Monday, 11 April 2022 00:00
Heel Pain Can Be Treated!
Tuesday, 05 April 2022 00:00
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Tuesday, 05 April 2022 00:00
What Causes a Bunion to Form?
 While the exact cause of a bunion is not always apparent, their bony disfigurement is hard to miss. Genetics are believed to sometimes play a role in the development of a bunion. Many consider gout and rheumatoid arthritis as a possible link to certain bunions that have formed, as well as abnormal foot structures such as flat feet, flexible joints, loose ligaments, and more. Tight, pointy high heels and other types of ill-fitting footwear may worsen a structural abnormality and increase the likelihood of a bunion forming. Standing for prolonged periods of time can also worsen bunion symptoms. Podiatrists deal with bunions every day and have various techniques for correcting them, depending upon how far along the deformity has progressed. Don’t delay in making an appointment with a podiatrist to have your feet examined if you have redness, swelling, soreness, an existing bony bump, or a bump that’s beginning to form at the joint of your big toe.
While the exact cause of a bunion is not always apparent, their bony disfigurement is hard to miss. Genetics are believed to sometimes play a role in the development of a bunion. Many consider gout and rheumatoid arthritis as a possible link to certain bunions that have formed, as well as abnormal foot structures such as flat feet, flexible joints, loose ligaments, and more. Tight, pointy high heels and other types of ill-fitting footwear may worsen a structural abnormality and increase the likelihood of a bunion forming. Standing for prolonged periods of time can also worsen bunion symptoms. Podiatrists deal with bunions every day and have various techniques for correcting them, depending upon how far along the deformity has progressed. Don’t delay in making an appointment with a podiatrist to have your feet examined if you have redness, swelling, soreness, an existing bony bump, or a bump that’s beginning to form at the joint of your big toe.
If you are suffering from bunion pain, contact one of the podiatrists of JE Foot & Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Fleming Island and Palm Coast, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Featured Articles
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019



